Groin pain in sportsman

|
What is groin pain and why is it often difficult to identify and treat? Some useful hints from our physiotherapist |
A BIT OF INFORMATION
How is it that still today groin pain is in many authors’ opinion one of the more investigated and less understood subjects of modern sports medicine? The secret is hidden in the term itself.
“Pubalgia” (from Latin “pubis” and Greek “algos”) literally means “groin pain” and, therefore, cannot indicate a pathology but just a symptom.
The latest definition was given by Busquet in his book “Le catene muscolari 3. La Pubalgia”: “the appearance of localised symptoms at the level of the pubis with pain irradiating to the adductors, abdominals and inguinal ligaments”; the author continues by stating that “ the diagnosis of groin pain is but an ascertainment, in that it doesn’t explain the cause. In the field of sport, groin pain is one of the more controversial diagnoses, not so much for the identification of the symptoms, but for the determination of the causes of the injury experienced by the patient”. That is the crucial point: to correctly identify the cause in order to correctly treat the pathology. This is far from obvious, and Jarvinen et al, 97 , have identified up to 72 different clinical entities, most of which concern muscular-tendon and osteo-articular disorders, but also infectious, vascular,or tumoral pathologies, bursitis, nerve entrapments, and others. All of this only confirms the fundamental importance of a correct diagnosis as an essential condition to plan a rational and effective treatment of the injury.
ANATOMIC HINTS
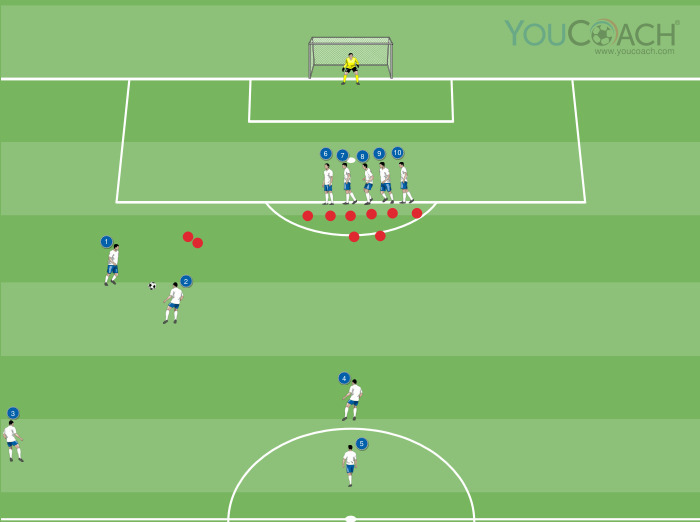
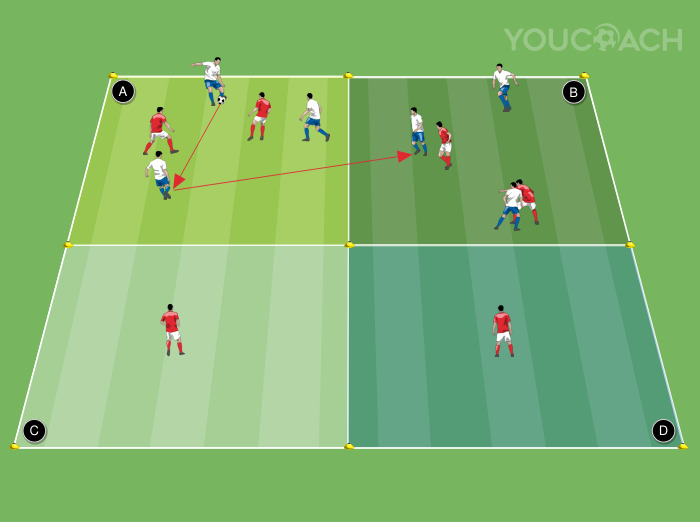
The pelvis (Fig.1) is a large, closed osteo-articular ring forming the lower part of the trunk; it forms the abdominal structure and connects the lower limbs with the spine. It is delimited by four bones: two hip bones joined centrally by the pubic symphysis and separated dorsally by the sacrum, with which they are articulated, and the coccyx. The pelvis includes four joints: two sacroiliac joints, the pubic symphysis and the sacrococcygeal joint.

Fig. 1: Pelvis
(A)Hip bone; (B) Pubic symphysis; (C) Sacrum; (D) Coccyx
 |
 |
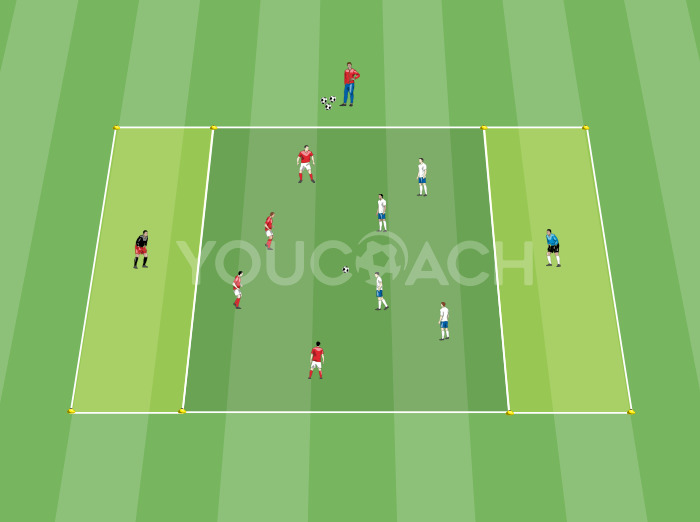
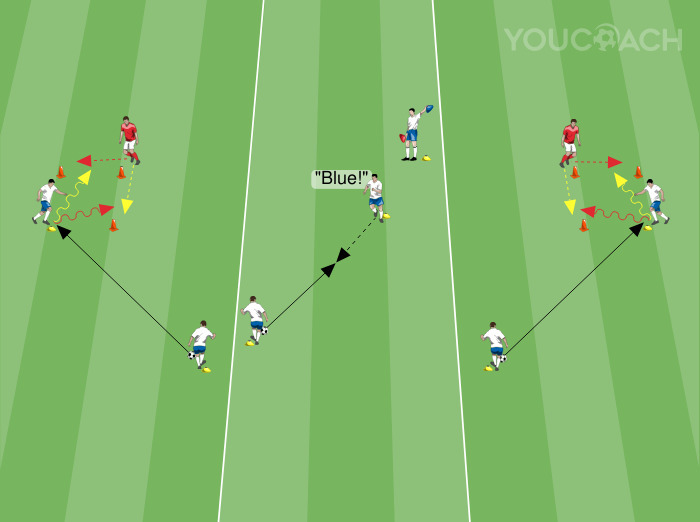
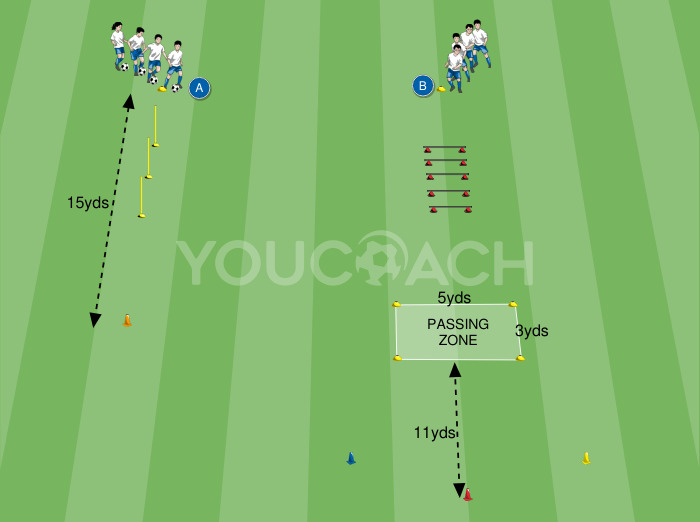
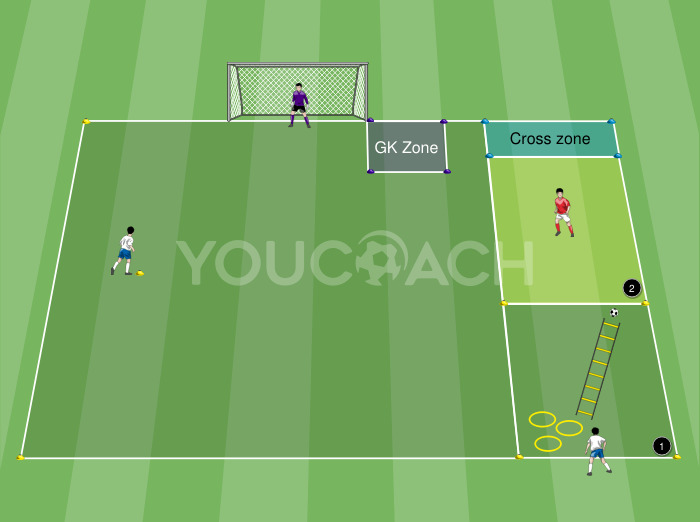
| Fig. 2. Pelvis muscles. Front view. | Fig. 3. Pelvis muscles. Rear view. |
Fig. 2: (A) Rectus abdominis; (B) Iliopsoas; (C) Abductors (tensor fasciae latae), (D) Adductors; (E) Quadriceps.
Fig. 3.: (A) Glutus medius (over the Glutus minimus); (B) Ischio-tibials; (C) Gluteus maximus.
PUBALGIA IN FOOTBALL PLAYERS: AETIOLOGY, TECHNICAL MOVEMENTS AND PREDISPOSING FACTORS
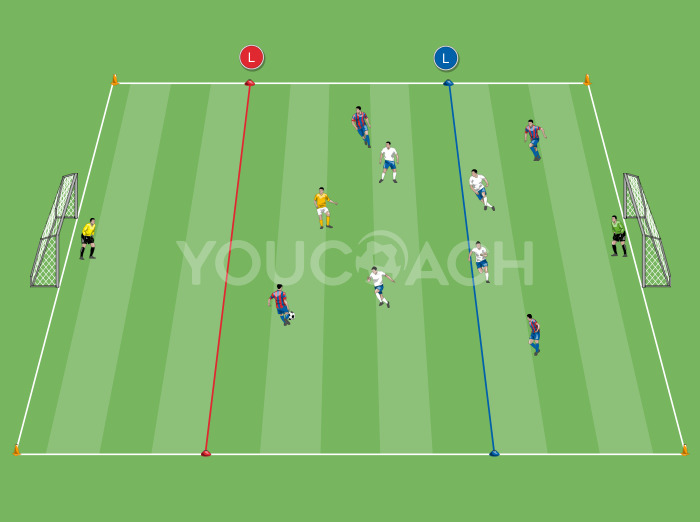
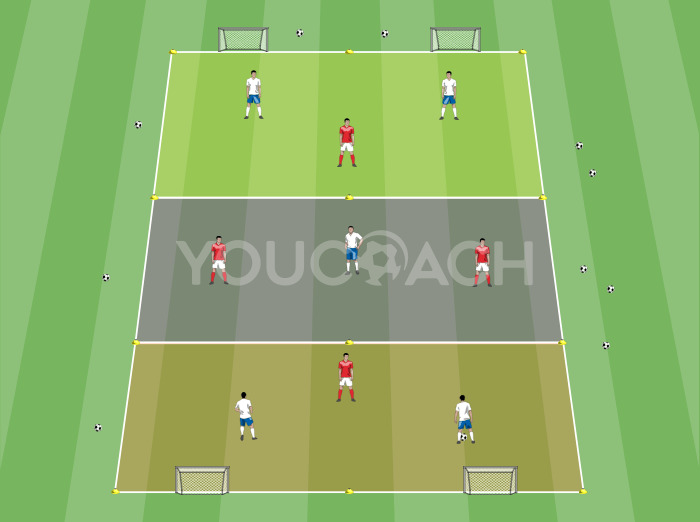
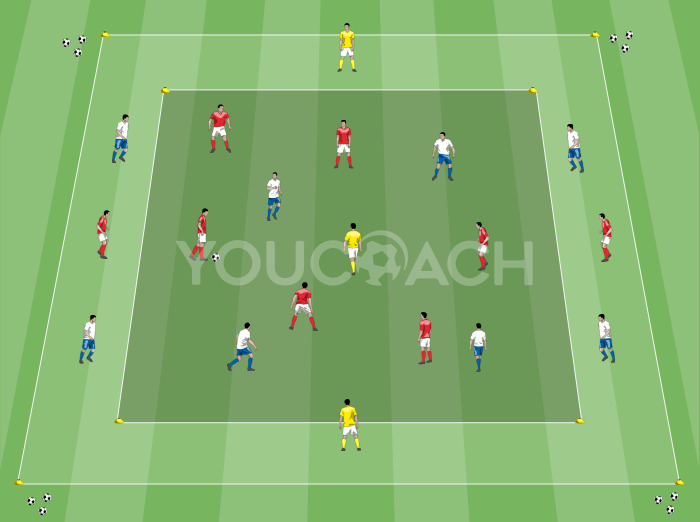
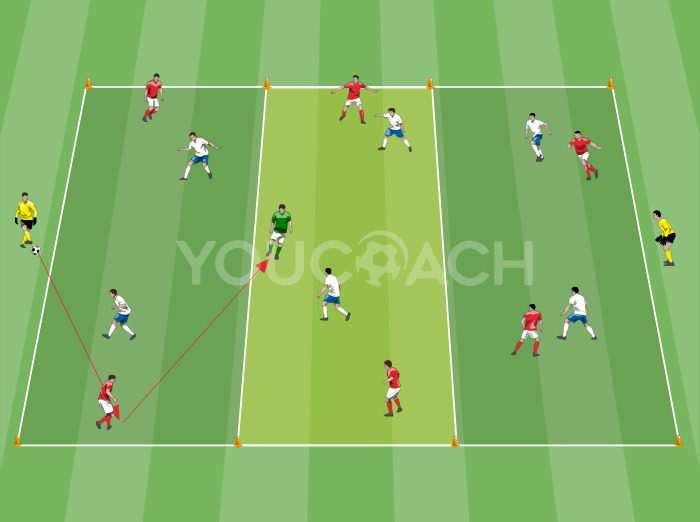
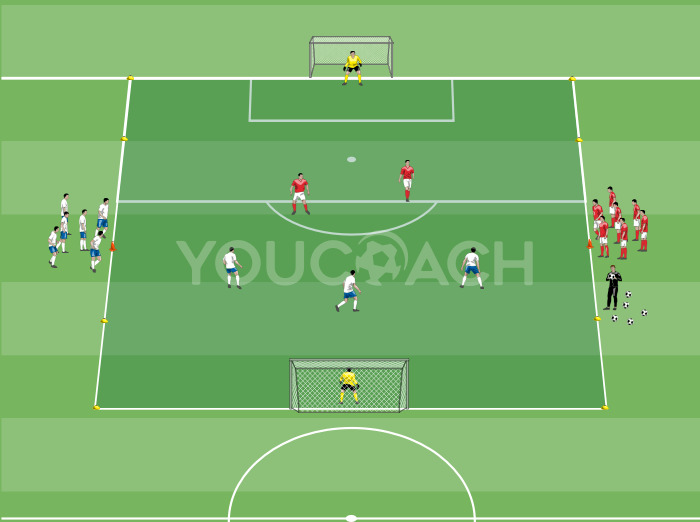
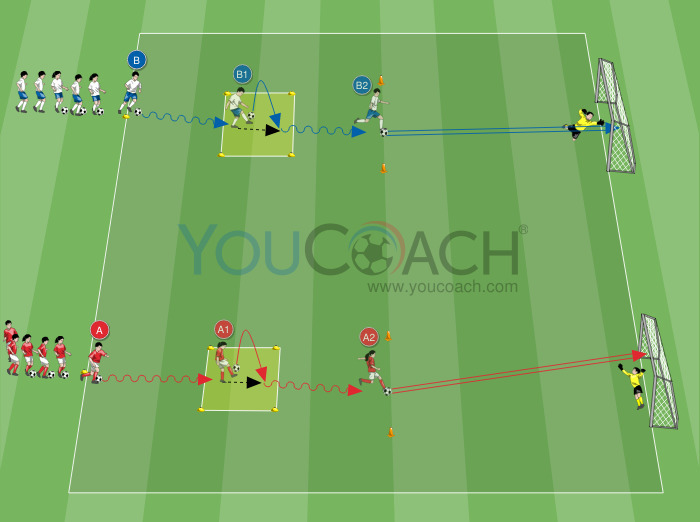
According to the literature, injuries of musculoskeletal or bone-ligament origin revealed by groin pain represent 5.18% of all injuries occurring in football. Let’s see why this figure is so high. Football includes many technical movements that can favour the symptoms: jumps, dribbling, changes of direction, slide tackle, are all factors that cause considerable strain in the pubic symphysis zone.
In his interesting study Busquet (1998) underlines that many years before pubalgia arises in football players, certain compensations can be perceived, mainly during kicking. In the author’s opinion, a good kicking technique requires that:
- The landing leg and the pushing leg are straight
- The flexion angle of the hip is considerable
- The more the posterior chain is extensible, the more the hip movement is free
This freedom provides a good ball control with loose, ergonomic and effective movements.

It is important to emphasize the enormous work done in these compensations by the abdominals (they contribute to the lifting of the pubic branches in the swing of the kick, to the dropping of the shoulders and a lumbar kyphosis as well), the iliopsoas (which performs the rapid flexion of the hip in synergy with the rectus femoris) and the adductors. The excessive work of these muscles causes:
- Susceptibility of these muscles: contractions, strain, lacerations;
- Inflammation;
- Pubic pain
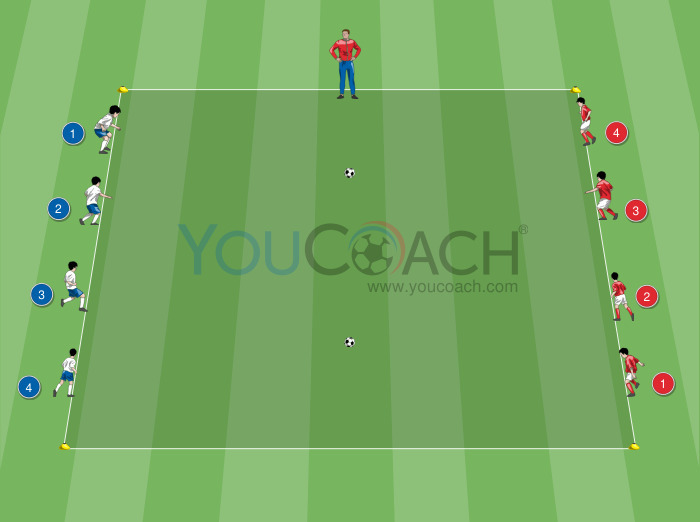
A long series of intrinsic and extrinsic factors that favour the onset of the symptoms has to be added to the above remarks. According to Bisciotti, possible intrinsic factors are:
- A clear asymmetry of the legs;
- An excessive lumbar lordosis;
- A functional imbalance of abdominal and adductor muscles, i.e., when abdominal muscles are weaker than adductor muscles.
- A pathology of the hip or of the sacroiliac articulation.
Possible extrinsic factors include:
- Unsuitable materials used in the activity (uncomfortable shoes, iron cleats used on hard grounds, or rubber cleats on muddy grounds, etc.)
- Rough playgrounds
- Errors in exercise planning.
WHAT TO DO IF GROIN PAIN APPEARS
When groin pain appears the symptoms should not be underestimated (as it often occurs) and a competent doctor should be sought as soon as possible to perform a clinical evaluation of the injury and, if necessary to ask for specific tests. In the meantime, in many cases pain will be relieved with ice pack applications (at least twice a day for 15-20 minutes maximum) or non-steroidal anti-inflammatory drugs (on medical advice or prescription only). Complete rest is absolutely necessary at least until medical or physiotherapy evaluation, or until complete resolution of the symptoms.
TREATMENTS
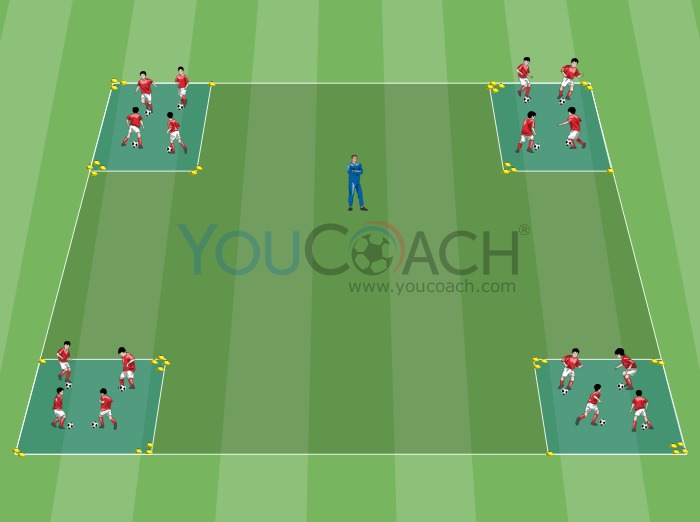
The first approach is a conservative management that consists of an initial period of rest or limited activity, drug therapy and physiotherapy. Physiotherapy may include physical treatments (electrotherapy, laser treatment), manual techniques for the treatment of soft tissue and joint structures such as manipulations or mobilization (Weir 2011, Weir 2009), exercise therapy to increase strength and improve coordination of the muscles that stabilise the hip and pelvis (Weir 2011, Verrall 2007, Holmich 1999).
Recent literature reviews indicate that manual therapy permits a quicker return to activity than exercise therapy; anyway, patients performing exercise for reinforcing abdominal and adductor muscles, stretching and functional exercises for the stabilization and coordination of the pelvis obtain better results than those receiving manual therapy (Almeida 2013, Marcon 2015).
if the results obtained with the conservative approach are not satisfactory non-steroidal anti-inflammatory drugs are used, steroids and/or prolotherapy (techniques including injection of drugs that stimulate the growth factors proliferation so as to promote tissue healing). If the symptoms do not disappear, surgery becomes necessary and heals about 90% of cases.
BIBLIOGRAPHY
- Almeida MO e coll. 2013, “Conservative intervention for treating exercise-related muscolotendinous, ligamentous and osseous groin pain”;
- Bisciotti N. 2009, "La Pubalgia dello Sportivo, Inquadramento clinico e strategie terapeutiche";
- Busquet L., 1998, "Le catene muscolari vol. 3, La pubalgia";
- Holmich 1999; “Effectiveness of active physical training as treatment for long-standing adductor-related groin pain in athletes: randomised trial”;
- Marcon F. 2015, “Revisione della letteratura con metanalisi sull'efficacia della terapia manuale e dell'esercizio terapeutico nel trattamento della pubalgia nello sportivo”.
- Paajanen 2011; “Laparoscopic surgery for chronic groin pain in athletes is more effective than nonoperative treatment: a randomized clinical trial with magnetic resonance imaging of 60 patients with sportsman’s hernia (athletic pubalgia)”;
- Passigli S. 2006; “Pubalgia e disfunzioni strutturali nel cingolo pelvico: valutazione e trattamento”;
- Verrall 2007 “Outcome of conservative management of athletic chronic groin injury diagnosed as pubic bone stress injury”;
- Weir A. 2011;“Manual or exercise therapy for long-standing adductor-related groin pain: a randomised controlled clinical trial”;
- Weir A. 2009; “A manual therapy technique for chronic adductor-related groin pain in athletes: acase series”.